
Dr. Mike Miyasaki
During this year we have seen many fantastic aesthetic cases performed by the PAC course doctors and faculty created by the Corr Dental Designs. Improved aesthetics can be a wonderful service we can provide to our patients, and besides how comfortable we keep them, the appearance of our work is probably one of the most important ways our patients judge our work and skills. But we know we have to develop aesthetics that function for the best cosmetic result and longevity. The PAC has spent hours this year to provide education on occlusion and function. What makes the PAC education unique is that we understand how to work with the most popular occlusal philosophies and allow the doctors to work up their cases in the manner they feel most proficient. What we ask is that they take the time to do a comprehensive examination, and if there are signs of occlusal instability (figures 1 and 2) that they inform the patient.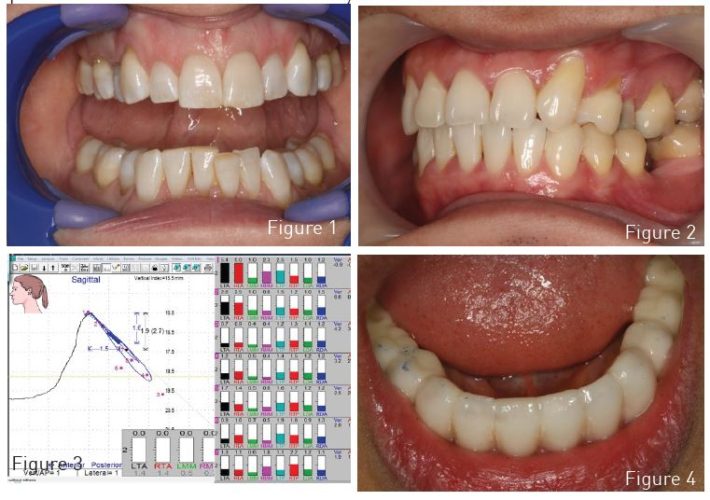 If the patient doesn’t value treating the functional challenges then we let the patient know the risks of doing so. If the patient wishes to address the functional issues we ask that the case is stabilized before moving onto the definitive restorative stage and that this is the most conservative option we choose with our informed patient. I feel this is a good approach to responsible dental care and I emphasize ‘care’.
If the patient doesn’t value treating the functional challenges then we let the patient know the risks of doing so. If the patient wishes to address the functional issues we ask that the case is stabilized before moving onto the definitive restorative stage and that this is the most conservative option we choose with our informed patient. I feel this is a good approach to responsible dental care and I emphasize ‘care’.
In the month of November, we were able to demonstrate the use of bioelectric diagnostic equipment at the course taught in Detroit led by Dr. Robert DiPilla. Using Myotronic’s equipment we presented what I think was a thought provoking experience for those in attendance to see how jaw position affected the muscle activity generate at rest, in maximum intercuspation, and in function. We were able to see how in space we could pick points where we could obviously see where the muscles were the most comfortable and move the patient’s mandible to that position to take a bite record (figure 3). How many times have we all taken a ‘bite’ by having the patient move to a position that looked ‘right’. Sometimes that bite ‘worked’ and sometimes it didn’t. Sometimes ‘worked’ meant the patient could bite down and hit all the teeth evenly, but to get into that position was the mandible in a truly physiologic position or was the patient having to adapt their jaw position (the moving part of the stomatognathic system) to accommodate closure into MIP? And over time would this develop into a bruxing problem or cause our patient to develop headaches from the muscle hyperactivity of going to this adapted position thousand times a day?
In my June PAC newsletter article, I showed the removable orthotic which is what I often choose to use when I first begin treating a patient. Dr. Robert Jankelson told me he felt he was able to equilibrate the removable orthotic the best because it could be removed from them the mouth and adjusted with the best of visibility. But with a removable orthotic the patient may be in their ideal physiologic position and yet the best healing may not be able to be achieved because when the orthotic is removed the joints and muscles go back into their pathologic position. This does not happen with the fixed orthotic (Figure 4) because it is left in the mouth 24/7. Once you have the proper maxilla-mandible orientation (Figure 5 and 6) the laboratory will do a diagnostic wax-up and create a putty stent that is used in the same manner the PAC teaches during the fabrication of their temporaries. In this fixed appliance adjustments are seen as a sign of healing and when a stable bite is established Phase II options can be considered.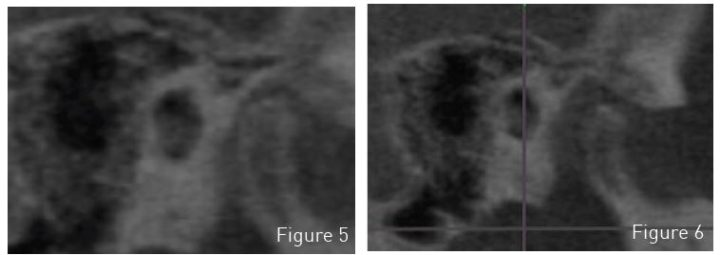
Following a system like this allows us to work better with the laboratory and establish longer lasting cases with improved aesthetics to truly improve the lives of our patients.
If you have questions about this article or if you would like to send a case, please contact the Pacific Aesthetic Laboratory Group at www.pacificaestheticdentalstudio.com, Gary Vaughn, CDT, CTO (916) 786-6740, or via email [email protected].
Figure 1. Teeth that have occlusal attrition or wear
Figure 2. Teeth that have abfraction lesions due to posterior interferences in lateral movement
Figure 3. Plotted jaw position with EMG’s
Figure 4. Fixed orthotic
Figure 5 and 6. Cone beam of condylar position pre-operative and post-operatively
