
Dr. Mike Miyasaki
At the time of this writing we have just concluded the preparation session of our full-mouth rehabilitation course in Denver. What an amazing group of clinicians, team and patients. It was an honor for me to work with them the past couple of days, and I look forward to seeing them finish their cases. Let me explain my definition of ‘full mouth therapy’. It is the establishment of a healthy stomatognathic system, creating health and stability and if restorations are needed, to do so in a conservative and aesthetic manner. It does not mean our objective is restoring the mouth with 28 restorations; in fact in the case described below the case was handled very conservatively.

Figure 1. The patient presented with a ‘normal’ looking bite.
In this newsletter I would like to discuss a case I presented to them as this case is an example of how we show patients what is going on, how we can recommend treatment that is very affordable and use this approach to attain the health and stability that we desire. In this case we saw a new patient who was suffering from headaches, joint pain and limited opening (figure 1). Her past clinicians had given her muscle relaxants which debilitated her, and recommended surgery and Botox neither of which she choose to do.
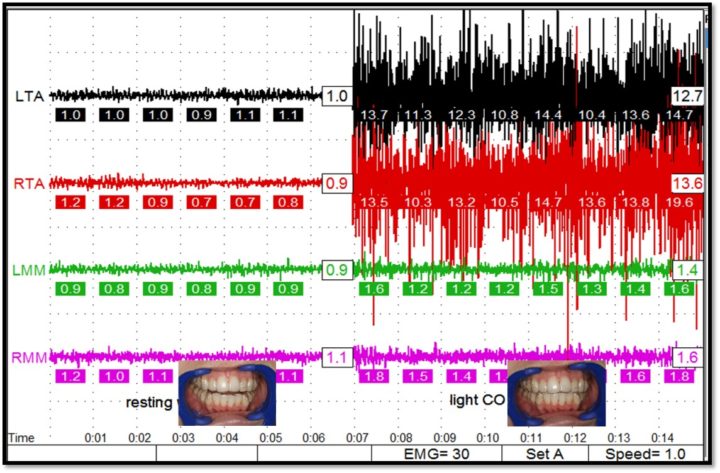
Figure 2. Left side shows normal tonus and low EMG’s. Right side shows when teeth are brought together increased EMG activity.
It is often the education of the patient that creates value for treatment. We used our bioelectric diagnostic equipment to show her that the cause was muscular hyperactivity and fatigue because of her malocclusion. We had her rest her mandible and recorded the temporalis and masseter emg’s which should be 2 mV’s or less in normal tonus. She was below 1.0 mV so well in the normal range (left side of figure 2).
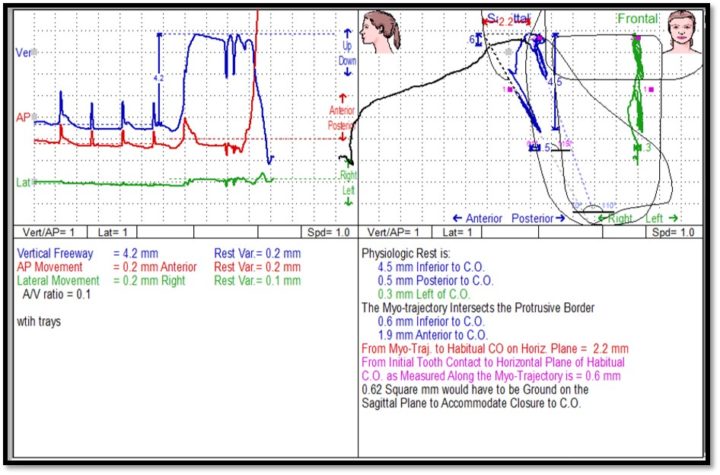
Figure 3. Shows the mandibular retrusion of 2.2 mm needed to achieve maximum intercuspation
But when we had her bring her teeth together in a light CO we could clearly show her that her muscle activity increased 1,200% when it should have had little or no change. Then using jaw tracking and real time EMG recording we were able to show her that from her physiologic bite position to her habitual CO she was having to retrude the mandible 2.2 mm which raised the activity of her temporal muscles. We were able to show her that the cause of the pain was her bite and she felt very comfortable with this having seen objective measurements.
The recommended treatment would be a lower removable anatomic orthotic that Corr could make for her. This would allow us to use a reversible treatment modality to show we could improve her pain.

Figure 4. An anatomic lower removable orthotic
There are different orthotics which fall into the broad categories of fixed and removable. Uses for orthotics are:
- To evaluate our ability to correct tooth W:L ratio
- To evaluate the corrections of facial esthetics
- To de-torque the mandible for better healing
- To reposition the condyles for better healing
- To remove deflective tooth contacts that often distalize or displace the mandible
- Reprogram CNS engrams by changing the occlusal proprioception
- Create an adjustable surface we can add or subtract from to promote healing
- Act as a prototype of the proposed occlusion and to see if improvements to occlusion are worth pursuing in multi-factorial pain cases
There is so much we can do when our patients have an appreciation for the stomatognathic system and how it works. And many times our treatment can be very simply done. I hope to see you at a PAC course soon so we can discuss this further.
If you have questions about my article or if you would like to send a case, please contact the Pacific Aesthetic Laboratory Group at www.pacificaestheticdentalstudio.com, Gary Vaughn, CDT, CTO (916) 786-6740, or via email [email protected].

