Dr. Michael Miyasaki
Ever have the patient with a very deep bite that is interested in aesthetic treatment (Figure 1)? You can restore them to their current habitual bite, but their facial aesthetics will be compromised with the lower third of their faces having a decreased vertical measurement. The decreased dental vertical dimension often will lead to displaced condyles and hyperactive accommodating muscles. And, finally, we often see that deep bites and breakage often go hand in hand.
When I have taught The PAC courses I have shared the philosophy of setting up the case to a point of occlusal stability and from there reconstructing the case to the desired aesthetics and function. The function is evaluated, a treatment plan is created, the endpoint is proven in Phase I orthotic use which allows for healing of the stomatognathic system. Finally once confirmed the case is predictably restored.
Let’s break this down. I use bioelectric diagnostic equipment made by Myotronics. After doing our comprehensive clinical examination (which includes photos and models) we determine the need to use the equipment to assess the patient, relax and deprogram the musculature and nervous system, and determine the best bite position that allows for seated joints and relaxed muscles. The vertical dimension is determined using smile design principles and the Golden Proportion to restore facial and smile aesthetics, and often improve the airway.

Figure 1
The scan (Figure 2) helps us assess the mandible’s position as the patient closes. Point A is where the muscles and joints would like the bite to be and Point B is where the teeth are guiding the muscles and joints which are now having to accommodate to maximum intercuspation. In this case the computer shows that the mandible is having to retrude 3.2 mm to accommodate this closure. This may be displace the condyles and cause the muscles to contract to retrude the mandible and hold it there.
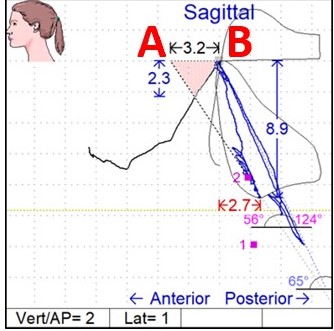
Figure 2
Using surface EMG’s we can see in Figure 3 that the muscle activity in the first third of the scan shows relaxed muscles, as the teeth are apart. In the middle of the scan we have relaxed muscles as the patient closes into our bite registration, our Myobite. And at the end of this scan we can see the EMG activity of the anterior temporalis muscles go up (all the color seen on the top two lines on the upper right) as the patient closes into their habitual bite and the mandible is repositioned.
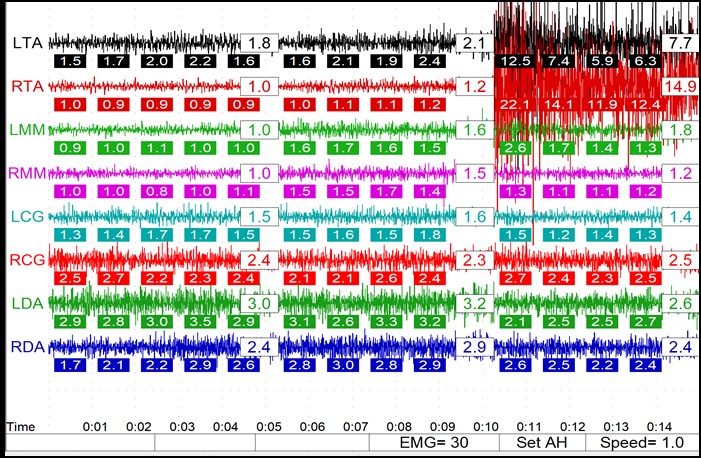
Figure 3
With diagnostic casts literally in hand (Figure 4) one can truly evaluate the occlusion in a way that might not be captured in photographs, and verify what we see is reflected in our scans. The maxillary central incisors are in lingual-version which is retruding the mandible.
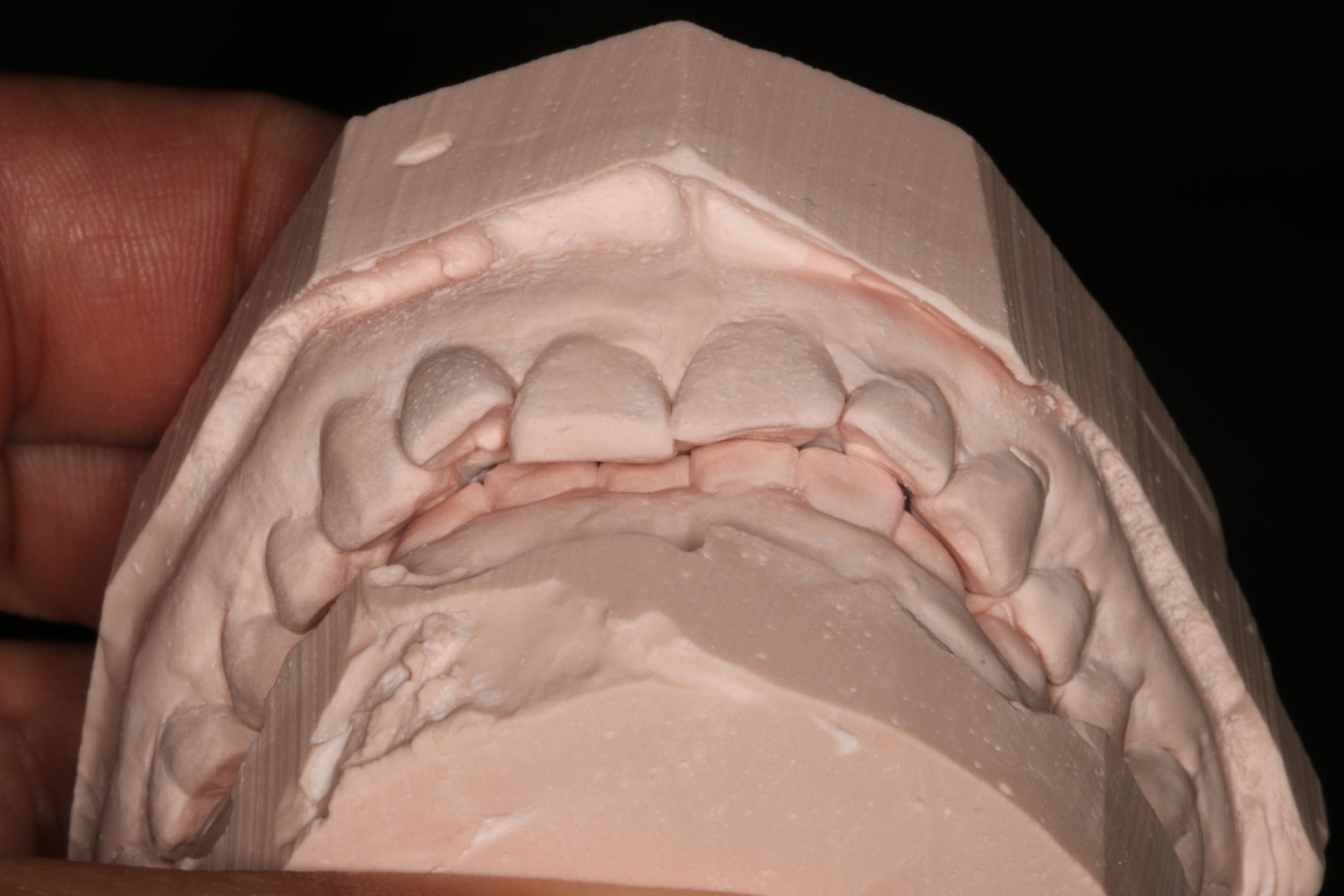
Figure 4
Our initial plan is to allow for healing by placing the patient in a segmented lower aesthetic mandibular orthotic made by Myoaligner (Figure 5). But while the lab was fabricating the orthotic we placed the patient in brackets and wires on the maxillary arch using the Cfast system to move the central incisors facially and round out the upper arch to lessen the mandibular constriction.

Figure 5
Figure 6 shows two of the three pieces of the removable Myoaligner orthotic in place and the middle anterior section removed so the vertical dimension change can be observed. The vertical dimension is therapeutic, functional, aesthetic and restorable. You might think the orthotic makes the teeth appear too long, but it should be remembered that this vertical change will be distributed to both the maxillary and mandibular arches.

Figure 6
When we had the mandible in the correct position we elected to intrude tooth #8 to match the CEJ heights of #8 and 9. When planning out the end result of adult orthodontics I like the soft tissue to be symmetrical. Although this might mean the incisal edges will not match, our aesthetic restorations will be correcting this discrepancy.
Figure 7 shows a scan taken after the orthodontics had moved the maxillary teeth facially and we can see that the mandibular constriction is reduced. This new scan shows that our bite is right where it needs to be. The computer showing 0.2 mm discrepancy is clinically acceptable, and more change may occur as more time allows for more healing.
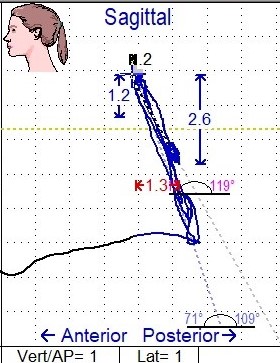
Figure 7
This case will be restored in a three-day over-the-shoulder course I will be doing along with Gary Vaughn, and if you attend a PAC course I hope to show you how this case progresses. The take away message is you can see how the planning was done for the final aesthetics and function. Time was allowed for healing, and the plans were made to conserve tooth structure by moving the teeth allowing the preparations to be done more conservatively. Stability was established and now we just have to manage the case as we teach in the PAC courses. We teach as we would like to be treated.
If you have questions about my article or if you would like to send a case, please contact the Pacific Aesthetic Laboratory Group at www.pacificaestheticdentalstudio.com, Gary Vaughn, CDT, CTO, (888) 461-3331, or via email gvaughn@thePAC.org.
