
Dr. Michael Miyasaki
I placed my first zirconia restoration almost 20 years ago. We were excited to have an aesthetic material that could be used for multiple-unit restorations. Zirconia could resist crack propagation and it was strong (Figure 1).
The initial trials we did were impressive because we were using such new technology. The restorations were milled from a block of zirconia that was scanned before it was milled. Each batch of zirconia would shrink about 20% when sintered so you would scan the block and the computer would figure out how to compensate for the shrinkage; meaning it would mill the restoration proportionally larger so when it shrank it had a precise fit (Figure 2).
CEREC was still evolving so we had to learn that because the restorations were milled, we had to be sure that all the internal line angles and corners were rounded and not sharp with about 6 degrees of taper (Figure 3). If you left sharp angles the CAD/CAM would compensate for it not being able to mill that sharp angle with its milling burs, and the restoration might even rock a bit, due to the ‘loosened’ fit.
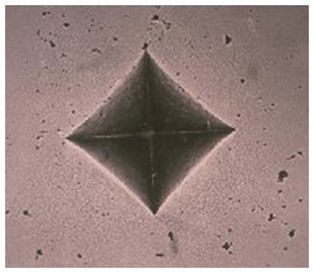
Figure 1

Figure 2
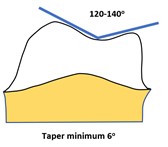
Figure 3
And then there were the aesthetics or lack of. You could effectively block out a black tooth preparation because the zirconia was so opaque (Figures 4 and 5).
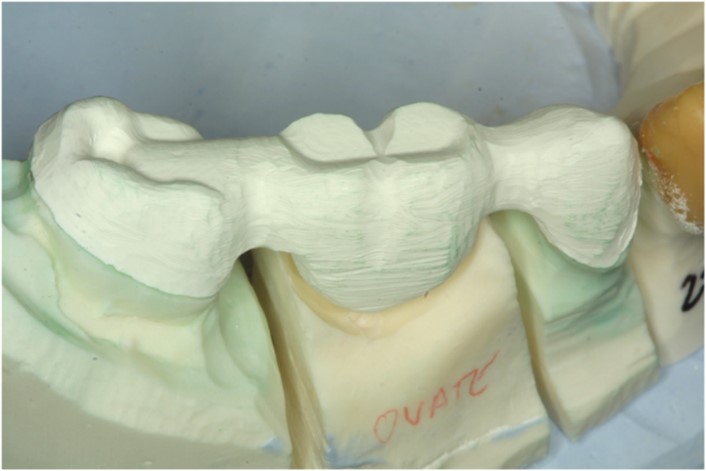
Figure 4
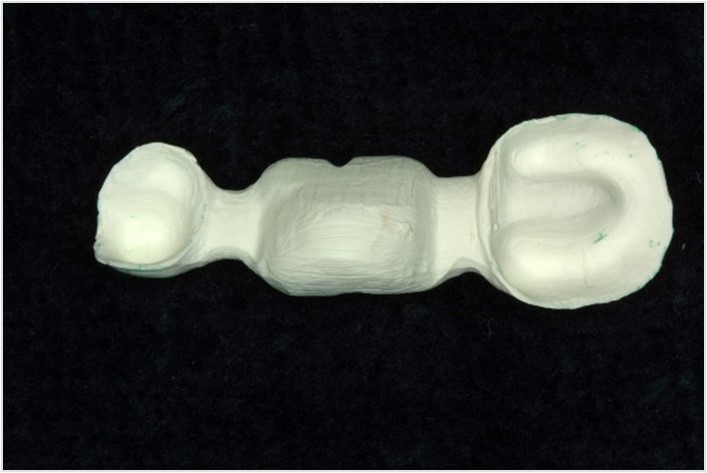
Figure 5
The opaque framework was then covered with a porcelain (Figure 6) like a porcelain-fused-to-metal restoration and because the coefficients of thermal expansion differed then layered porcelain would often separate from the framework.

Figure 6
And then if we bonded this wonderful restorative material (said sarcastically) it would often debond if we did not have enough mechanical retention. We didn’t realize the saliva contaminated the internal surface so that bonding the restoration in was ineffective. I have written it here before; I was not a big proponent of the material. But this old dog can learn new tricks. That was then, and thankfully, the materials and I have improved.
Where are we now? The material is now much more aesthetic when fabricated by a skilled laboratory, such as Corr Dental Designs /Pacific Aesthetic Dental Laboratory. The material is stronger than e.max and can be bonded for retention as long as you use a zirconia cleaner and zirconia primer before bonding (personally I use Vista Apex’s ZR-C and ZR-P which have been shown to be the most effective cleaner and primer on the market, currently, but I am biased).
Personally, I will typically use zirconia-full contour for the restorations from the first bicuspid back (maybe from the second bicuspid) and zirconia-layered restorations in the cuspid-to-cuspid region (Figure 7). I feel there is less chance of failure when using solid zirconia, but where aesthetics need to be considered a layered restoration provides a very nice aesthetic result.

Figure 7
Here is a case that was recently completed (Figure 8). The maxillary teeth needed restoring and the lower had a removable prosthesis. We first determined the proper vertical dimension and I mounted the models with the mandibular arch in the desired position. I then did a quick wax-up to fabricate an acrylic overlay over the non-prepared teeth to show the patient what we could do. This was the key motivator. But I made a putty matrix off the wax-up and placed it over the teeth so I could visualize the preparations (Figure 9).

Figure 8

Figure 9
The laboratory fabricated beautiful zirconia restorations with layered zirconia in the anterior. What makes them look so nice are the contours and embrasures (Figures 10 and 11).
Figures 12, 13, 14, and 15 show the pre-operative and post-operative results attained on the upper arch with zirconia crowns on teeth #4-14. With this one material, we have attained fantastic aesthetics and restored the occlusion. I feel this case is going to have a lot of longevity.

Figure 10

Figure 11
Zirconia is a material that like all the others needs to be understood and used in the proper situations. Remember when you lack the mechanical retention you need to bond them in properly. The results can be life-changing.

Figure 12

Figure 13

Figure 14

Figure 15
If you have questions about my article or if you would like to send a case, please contact the Pacific Aesthetic Laboratory Group at www.pacificaestheticdentalstudio.com, Gary Vaughn, CDT, CTO (916) 786-6740, or via email [email protected].
