
Dr. Michael Miyasaki
I am always amazed by the skills displayed by the doctors who show their work in this newsletter. All the step-by-step instruction makes this newsletter interesting to read. A shout-out should go out to Rae Rankin, the one who coordinates, edits and layouts each issue. As part of the team, Rae makes this information presentable and usable. We have to recognize the effort and appreciate what this teams gives to us the reader.
Now I switch from reader to sharer, and this month I wanted to show a case done by Ryan Corr that for me illustrates what we talk about when doing larger cases and the need to work with a laboratory that understands the principles to make the case successful from the aesthetics to the occlusion.
This case started out when the patient came in for an aesthetic consultation. I began by discussing with the patient what her wishes were. In this case her desire was for a nicer smile with white teeth and her questions were about veneers. I said veneers could be done, but I showed her that she had a 100% overbite (Figure 1). I explained to her this amount of overbite was much more than we typically desire. I pointed out that as her natural teeth had worn due to this bite situation that I would be concerned about something similar occurring again with just veneers. She also mentioned headaches and I explained that these could be exacerbated by her occlusion. Since we were talking about aesthetics, I also pointed out that with her deep overbite she had deeper folds at the corner of her mouth and thinner lips which gave her a more aged appearance. She agreed and asked what my recommendations would be.

Figure 1
I told her I would like to evaluate her occlusion and determine a better place for her lower jaw in relation to her upper teeth. And I explained that this new bite would put the jaw joints in a better position and would also allow the muscles in the head and neck to relax and maximize their efficiency in function (Figure 2). I explained that we would do this objectively using equipment to help us determine the correct position and I could then show her. I explained that a trial of this new bite would be done with the use of an orthotic that would place her jaw in this more ideal position (Figure 3). This orthotic provided us with a reversible beginning point and it could be easily adjusted until we confirmed the best bite for her from an aesthetic and functional perspective, and the patient agreed.
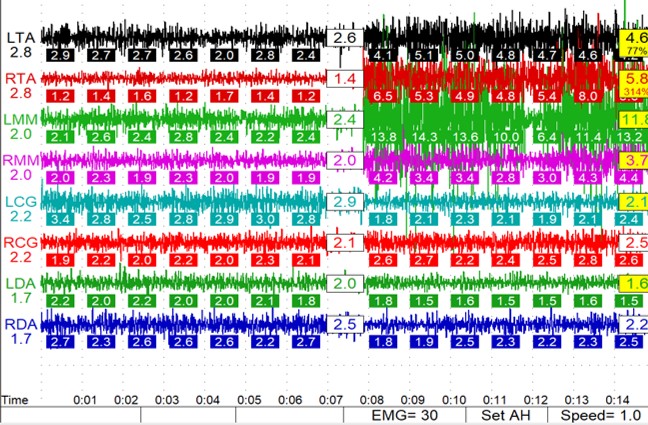
Figure 2
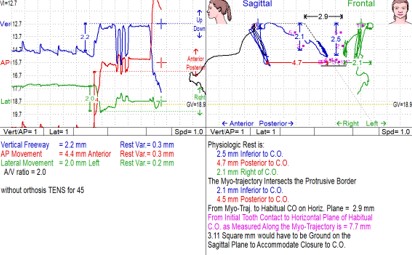
Figure 3
We then had a mandibular anatomic removable orthotic fabricated by Corr Dental Designs (Figure 4) to be sure she could function in this new maxillary-mandibular relationship. And for the next few months we adjusted the orthotic, if needed, and verified we had good occlusal stability and comfort. This was the diagnostic and healing period in this treatment. It reminds me of placing an implant and allowing it to heal and become stable before restoring. By doing this, we are allowing the muscles and joints to heal, and the CNS to develop healthy patterns and responses before irreversibly changing a tooth.

Figure 4
Pre-operative models were mounted with this newly verified occlusal relationship and a diagnostic wax-up was done (Figure 5). From this wax-up were developed the preparation stent, bite registration stent and temporization stents.

Figure 5
While we prepared all the teeth in one visit, we relined a bite registration stent in segments (Figure 6) while always having tripodized oral contacts, so we did not lose the occlusal relationship.
It is always so reassuring when we make the temporaries, and the bite is correct (Figures 7 and 8). This is a sign of exceptional laboratory work.

Figure 6

Figure 7

Figure 8
The laboratory then took the models of the prepared teeth and our relined bite registration stent and mounted the models. We call this ‘team bite management.’ And from these models, properly mounted, the final restorations were fabricated. When bonded in there was no significant adjustment needed. It is always hard to evaluate the case with the patient’s entire mouth numbed during the bonding, but at a subsequent visit, the patient gave me a hug and said she loved to smile.

Figure 9
I would like to thank the team at Corr Dental Designs and Ryan Corr for doing a job that put a smile on our patient’s face (Figure 9). Magnificent work! And I would love to learn from our readers – please share what you would have done differently.
If you would like to send a case, please contact the Pacific Aesthetic Laboratory Group at www.pacificaestheticdentalstudio.com, Gary Vaughn, CDT, CTO (916) 786-6740, or via email [email protected].
